Fatigue, brain fog, mood swings… you name it, I’ve had it.
For years I’ve felt ‘inflammed’. I knew I wasn’t well.
I just didn’t know why.
I told my doctors the same story every visit – I’m really tired. I can’t put my finger on it but I don’t feel right.
They all checked for the same issues over again – thyroid function, viral antibodies, blood counts, iron levels etc.
They also always checked my fasting blood sugar. It was always ‘normal’.
“Your bloods look great.” They would say.
“Maybe it’s lack of sleep, or stress….”
I would accept their diagnosis. I did lack sleep. I was stressed! I have 2 young kids who don’t sleep through the night. I have a demanding job.
This year, my symptoms escalated. My vision got worse and I crashed every afternoon from fatigue.
“This has got to stop!” I screamed in my head. Someone has to take the lead. Being a doctor myself, I know what goes through their heads when patients tell them they are ‘tired’. No doctor was going to delve further if the routine blood work looks OK. They just put it down to ‘stress’ or ‘crazy’.
I knew I was eating badly. I snacked throughout the day, ate more junk than I care to admit, and probably (definitely) ate way too much. Still, I prided myself on being a pretty good 41 year old. I’m 160 cm (5 ft 4 in) and weigh 50 kilos (110 pounds). My BMI comes in at a healthy 19.5 (Not that this matters. Lean people get diabetes too). My blood work has always been good and I’ve never been diagnosed with any disease, even during pregnancy.
I figured my bad diet is probably why I felt so bad.
But I couldn’t stop. I would vow to eat better every morning and ended up giving in multiple times during the day, escalating as I failed yet again to resist a cookie or a square of chocolate.
I’ve been listening to Mark Hyman and various other wellness podcasts. I knew about continuous glucose monitors (CGMs). Maybe seeing my blood sugar go up when I eat a muffin will be the wakeup call I need to stop eating badly.
Boy was I right.
Why is a Continuous Glucose Monitor (CGM) better than a fasting blood sugar (FBS)?

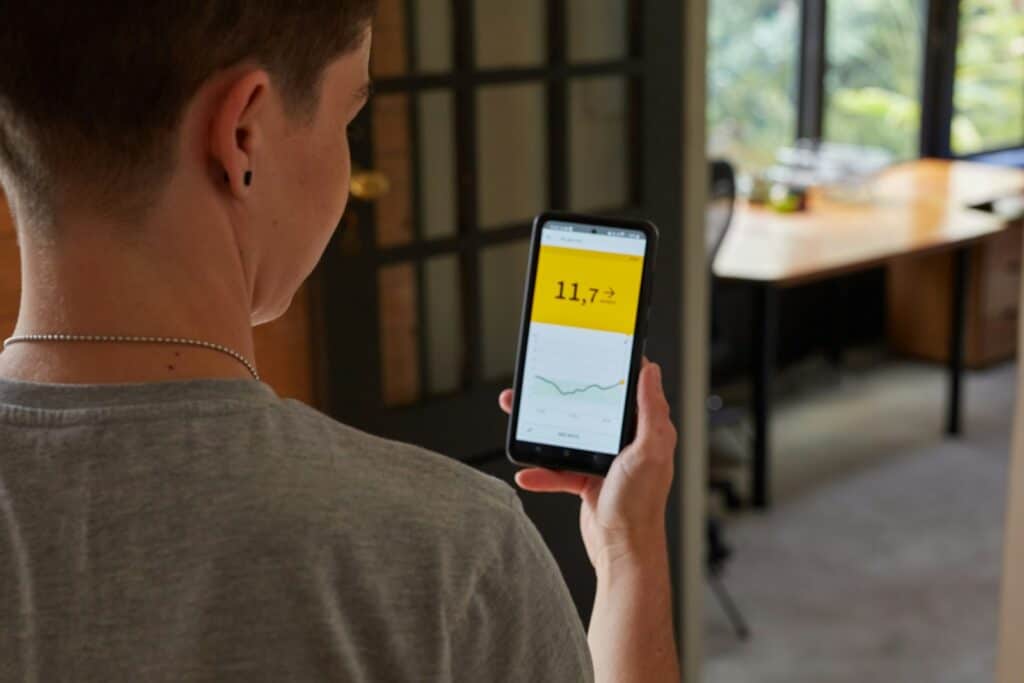
I stuck the CGM on in the afternoon after lunch. The monitor immediately picked up a blood sugar of 7.0. Not great, but not too bad for 2 hours post-meal. It’s still within the normal range. Then I ate a small handful of tortilla chips and it shot up to 8.0.
My appetite for chips disappeared.
Throughout the next 2 weeks, my trusty CGM told me my metabolic health was shit and proved to me that the foods I knew were bad, were indeed bad. Plus, a few I thought were good for health, like bananas. More on that in another post.
Because, right there, is why a CGM is light-years ahead compared to a one-time fasting blood sugar (FBS) when it comes to diagnosing diabetes. Your fasting blood sugar might look deceptively ‘normal’ but like me, your body could be struggling to process sugar when it floods your bloodstream.
The FBS gives you a snapshot of your blood glucose level at a particular moment, but it doesn’t provide any information to understand the patterns and trends in your glucose levels.
On the other hand, CGMs automatically measure your blood glucose levels throughout the day and night, providing a more comprehensive and real-time view of your glucose fluctuations. It even estimates your HbA1c after it gets enough information.
How do Continous Glucose Monitors (CGM) work?
Continuous Glucose Monitoring, or CGM, is a technology that allows you to monitor your glucose levels continuously throughout the day and night. A CGM system includes three parts: a tiny, disposable sensor inserted under your skin (your belly or arm), a transmitter, and a receiver displaying real-time glucose data.
The sensor measures the concentration of glucose in your interstitial fluid (not blood) and sends this data to a transmitter, which wirelessly relays it to a display device like your smartphone or a dedicated CGM receiver.
CGMs provide real-time glucose readings, trends, and alerts for high or low glucose levels, allowing you to make informed decisions about your diet, exercise, and insulin dosing.
What is Fasting Blood Sugar (FBS)?
On the other hand, fasting blood sugar refers to your blood glucose level after not eating or drinking (except water) for at least 8 hours. It’s a simple, single test done with a traditional glucose meter, measuring capillary plasma glucose concentrations.
Is a CGM or FBS more accurate to diagnose diabetes?
Although CGM provides more frequent data, it may not always be as accurate as doing a blood test, especially if the sensor or device experiences technical issues. Even with the newer CGMs, there can be a lag of 5-20 minutes before the CGM catches up to fingerstick (blood) sugar results.
However, when all its readings are taken as a whole, the CGM gives you a better overview of your blood sugar control, especially when food is involved. A FBS only gives you a snapshot of your blood sugar level when you haven’t eaten anything for 8 hours – practically useless to diagnose most people with pre-diabetes or early diabetes when your FBS is still in the normal range.
Is there an alternative to the CGM?
It’s obvious why a CGM is better at diagnosing diabetes, pre-diabetes, early diabetes and poor metabolic health than a fasting blood sugar. However, the cost for some can be prohibitive.
Is there a cheaper alternative to the CGM to get a better overview of your metabolic health than a FBS can?
Yes, but you may not like the answer.
You can use blood glucose monitors (like the Abott Freestyle Optimum Neo) and do a pinprick at different times of the day – mainly a fasting one, pre-meals, 1 hour post-meal, 2 hours post-meal, and randomly in between. When you take all these stand-alone blood sugar levels as a whole, you’ll see a pattern emerge. This is similar to what you will see with a CGM.
It works, but it hurts.
And you’ll probably find the total cost of the monitor and disposable strips isn’t that much lower than using a CGM for 2 weeks.
 Check it out on Amazon
Check it out on Amazon
